
PROSTATE CANCER CARE IN SINGAPORE
A Personalised, Non-Invasive Treatment For Every Stage of Prostate Cancer
WHAT IS PROSTATE CANCER?
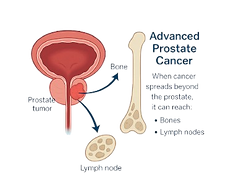
Prostate cancer begins when cells in the prostate – a small gland that helps produce semen – start to grow abnormally. These cells can form a tumour, which may stay localised or, in some cases, spread to nearby tissues or other parts of the body such as the bones or lymph nodes.
YOUR PROSTATE CANCER JOURNEY
From early detection to non invasive advanced cancer treatment, explore how each step — including latest interventions like SpaceOAR — contributes to a tailored prostate cancer care plan.
SCREENING & RISK ASSESSMENT
Prostate cancer often develops silently, without early symptoms. If left undetected, it may progress and spread, reducing treatment effectiveness. Screening helps detect prostate cancer before symptoms arise, improving outcomes and enabling timely, targeted care.
LOCALISED PROSTATE CANCER (EARLY STAGE)
Localised prostate cancer means that the cancer is contained within the prostate gland and has not spread to nearby organs, lymph nodes, or bones. It is considered an early and potentially curable stage of the disease where treatment is most effective.
For localised prostate cancer, Radiotherapy has been shown in a study with 15-year-follow-up to offer comparable cure rates to surgery (PROTECT). A recent advancement is Stereotactic Body Radiotherapy (SBRT) which allows radiotherapy to the prostate to be completed in just 5 sessions.
Recently published clinical trials have shown that Prostate SBRT was just as effective as standard radiation (PACE-B), and that it was associated with far less urinary incontinence and better sexual function than removal of the prostate (PACE-A).
These findings have positioned prostate SBRT as an option for men with early prostate cancer to avoid surgery, and get cure with minimal disruption to everyday life.
PROTECT: https://pubmed.ncbi.nlm.nih.gov/36912538/

RISK STRATIFICATION FOR LOCALISED CANCER
Risk stratification within localised prostate cancer is essential for guiding evidence-based, stage-appropriate treatment. A prostate oncologist plays a critical role in interpreting risk categories and developing tailored treatment strategies — helping to optimise curative outcomes while minimising unnecessary intervention.
LOW RISK
Low PSA
Low Gleason Score
Active Surveillance or SBRT
INTERMEDIATE RISK
Moderate PSA
Moderate Gleason Score
SBRT+/- Hormone Therapy
HIGH RISK
High PSA
High Gleason Score
RT + Hormone Therapy
ADVANCED & METASTATIC PROSTATE CANCER (STAGE 4)
In select Stage 4 cases, where prostate cancer has spread to only a few sites, SBRT can be used to target visible tumours in the bones, lymph nodes, or prostate with pinpoint precision. This highly focused radiation helps control cancer at specific sites, often delaying the need for long-term drug therapy. Like surgery, SBRT aims to destroy the tumour completely — but without incisions or hospital stays. Treatment is done in 1–5 outpatient sessions, offering a powerful and non-invasive tool in managing advanced disease.
Prostate SBRT (Stereotactic Body Radiotherapy) is a non-surgical treatment that uses advanced technology to deliver high-dose, precisely targeted radiation to eliminate prostate cancer cells. “Stereotactic” means the radiation is shaped and guided with pinpoint accuracy, minimising damage to surrounding healthy tissue. Once treated, the cancer cells stop growing and eventually die, with the body naturally clearing them away — offering an outcome similar to surgery, but without any incisions, pain, or hospital stay.

QUICK TREATMENT TIME
3-5 sessions, over 2 weeks
OUTPATIENT BASED
No hospital stay required
NO OPEN SURGERY
No cuts or stitches.
No operation risks.
Bloodless.

NO ANAESTHESIA
Comfortable and painless
SPACEOAR HYDROGEL: MINIMISING RADIOTHERAPY SIDE EFFECTS
Protecting What Matters Most During Treatment
SpaceOAR Hydrogel creates a protective space between the prostate and rectum—helping to reduce side effects and preserve quality of life during radiation therapy.
Speak with our Prostate Oncologists Today
DR JONATHAN TEH YI HUI
Medical Director (CSR), Senior Consultant Radiation Oncologist
MBBS (SIN), FRCR (Clinical Oncology, UK), FAMS (Radiation Oncology)
Dr. Jonthan Teh is Medical Director and Senior Consultant Radiation Oncologist at Centre for Stereotactic Radiosurgery (CSR), bringing with him over 20 years of experience in cancer care. Previously a Consultant Radiation Oncologist at the National Cancer Centre Singapore (NCCS), He was the principal investigator of a phase II trial in stereotactic ablative body radiotherapy (SBRT) for low-intermediate risk prostate cancer from 2013 to 2017, which was Southeast Asia’s first trial of this non-invasive treatment technique for prostate cancer. He is a first co-author of the publication documenting the efficacy and safety of prostate SBRT in the Singapore population in the Asia-Pacific Journal of Clinical Oncology.A leading expert in the treatment of prostate cancers, he is deeply committed to delivering precise, compassionate care to each of his patients.

DR DANIEL TAN YAT HARN (PBM)
Director, Senior Consultant Radiation Oncologist
MBBS (SIN), FRCR (Clinical Oncology, UK), FAMS (Radiation Oncology),
MBA (Healthcare Management)
Dr. Daniel Tan is Medical Director and Senior Consultant Radiation Oncologist at Centre for Stereotactic Radiosurgery (CSR), bringing with him over 20 years of experience in cancer care. Previously a Consultant Radiation Oncologist at the National Cancer Centre Singapore (NCCS), he was instrumental in developing the region’s first advanced Spine, Prostate, and Liver SRS/SBRT programs, pioneering their introduction in Southeast Asia. Dr Daniel’s radiosurgery expertise extends beyond the shores of Singapore. In June 2024, Dr Daniel was elected to the Board of Directors of the International Stereotactic Radiosurgery Society (ISRS), the world’s largest radiosurgery professional organisation.

Our Insurance Panel
Please reach out to us to find out more on financing your treatment
Stories of Hope

Gordon had been living a healthy, active life when he received news that would change his life as he knew it forever. Faced with a prostate cancer diagnosis, he was determined to nip the problem in the bud immediately. As an engineer by profession, his problem solving skills determined that the most efficient path to complete remission would be surgery. However, when he was presented with an alternative treatment - Spaceoar and Radiation therapy at Asian Alliance Radiation & Oncology - his perspective changed completely.
For some, cancer can be a defeating experience; for others, a victorious turning point. Approaching 60 and diagnosed with prostate cancer, the experience was the catalyst for a complete lifestyle change that Kelvin Tang never imagined, and the start of physical triumphs he could never have fathomed at his age.
About Asian Alliance Radiation & Oncology
Founded in 2015, Asian Alliance Radiation & Oncology (AARO) is Singapore’s first independent radiation oncology clinic which has since grown to become an Oncology Group with its own radiation treatment center, ‘Centre for Stereotactic Radiosurgery’ situated at Adam Road.
Anchored by a multidisciplinary team of Oncologists and Healthcare Professionals who are well-versed in the latest cancer treatments and trends, AARO aims to provide a one-stop solution for each patient’s unique situation – delivering evidence-based medicine and personalized care.















